 |
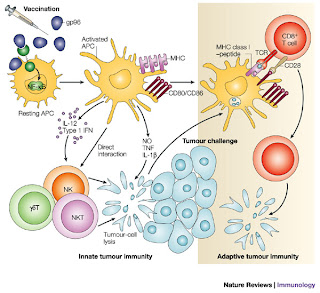
| Figure #1: Non-specific vaccine image(9) |
I tried to find the a published study that had inspired the many articles on this new vaccine. Unfortunately however, I could not find it, most probably attributed to the fact that this study is so recent. But I did find many websites that were advertising for patients with glioblastoma to participate in clinical trials (2). I also did find a link to where the study will be presented at the American Association for Clinical Oncology (8), therefore, I was less skeptical on the validity of the article I was reading. Fortunately, there have been studies conducted in relation to HSPPC-96 for melanoma (3)(4), renal cell carcinoma (5), pancreatic adenocarcinoma (6), and non-Hodgkin lymphoma (7). I also discovered that this drug has been formed after the discovery of cancer immunity caused by gp96, a polypetide which seems to be the cause of all this hub-bub.
What is HSPPC-96 and How does it work?
HSPPC-96 comes from a family of proteins that are referred to as heat shock proteins (HSP). HSP's are glycoprotiens which are the most commonly found proteins in living organisms. They provide a variety of functions which includes the involvement in the folding and the unfolding of other proteins. HSP's get their name because they are highly responsive to changes in temperature. In particular, when there is heat shock, the protein is known to be dramatically upregulated. (10)
 |
| Figure #2:HPPC-96 affects tumor cells (12) |
Nicchitta is not the only person who discusses the importance of this polypeptide. In most of the papers that I read, HSP is linked to activating gp96. gp96, is referred to as a tumor suppressing antigen, and it's properties and function in relation to cancer cells occurred in 1986 by Srivastava and colleagues. This research which was conducted determined that gp96 when isolated from tumor cells and injected into cancer free mice created an immunization effect. Later, when live cancer cells were added, the mice would not die from cancer (11).
What does this mean? Questions for Further Research.
The main questions that I had after this research were the following:
How does this effect surrounding cells, aka normal cells?
This question came from the fact that HSP proteins are one of the most prevalent proteins in living organisms. This then prompted the thought, if that is the case, then how does the activation of the CD91 receptor specifically attributed to cancer cells? Upon finding the study done by Srivastava on the tumor antigenic properties of gp96, I understood. In the research they found that gp96 that was isolated from normal cells did not work as an effective immunizer, that mice that were injected with the normal gp96 died from cancer after being injected with cancer cells. Therefore the vaccine could not effect normal cells because the vaccine itself is isolated from existing, or previously existing tumor cells from the patient. This explains the fact that the HSPCC-96 vaccine is effective only for patients that have already experienced glioblastoma which has metasticized. That way, scientists can isolate those individual's personal tumor genetic information and use it to create the vaccine.
Can there be a general vaccine developed for those who have not had cancer?
This question is still yet to be answered but my educated guess would be the following:
That a general vaccine may be developed in regards to specific mutations. As Dr. Islas mentioned, there are as many cancers as there are types of cells in the body. Thus, there would be the same amount of vaccines based on the research done so far. I think that most of us might agree that it would be a little overboard, to take vaccines for every type of mutation possible.
Based on these facts, then the general agreement would be that we would need a mega-cancer-vaccine, to solve this problem, obviously this has not been developed. Then comes an argument of whether cheating cancer is cheating death...but I'll leave that one for a separate post.
Conclusions and Reflections
This actually got me very excited. My cancer project is cancer and the immune system, and I was not anticipating that this article would lead to me finding out more about it.
It is clear that immunotherapy and the like has a lot going for it. Specifically the ability to create an HSPPC-96 virus which is created using the tumor cells of the patient. I was also surprised to find that a lot of this research has been done very early on in '74 the one of the first papers was published regarding the specificity of HSP receptors in relation to cancer.
Another surprise for me was the flexibility of this vaccine, specifically the fact that researchers have applied it to a variety of different cancers with relative success.
In my humble opinion, I really think that immunotherapy is the way to go to cure cancer. I feel that it is much more safe and successful and less "invasive" if you will. That in a way we are supplying the immune system with the needed artillery to fight the battle and win it, that way not only is the cancer gone, but it has a very small likelihood of entering remission because your body has been vaccinated against it.
The drawback of this of course, is that this vaccine works only in cases in cancers that have already been found and in all most all cases have metasticized. Thus, this is not a preventative vaccine against cancer for life. They do not create ways for normal cells to be protected from becoming or evolving into cancerous cells.
However, these vaccines I feel, are the first steps towards creating preventative vaccines for cancer like the chicken pox or measles. Obviously of course, there are repercussions just as there is for any medicine. But in the end, I feel that this definitely a step in the right direction, and certainly makes me hopeful!
